Abstract
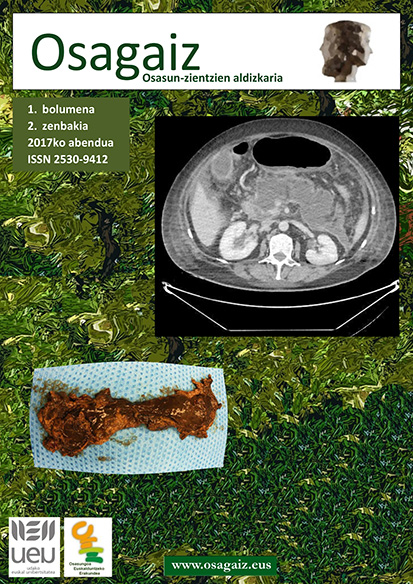
Acute pancreatitis is an acute but benign disease of the pancreas. It is usually a mild illness, but in its most severe forms mortality and morbidity can be high. For these severe forms of the disease, it is very important to have a multidisciplinary protocol for clinical management at the different levels of assistance. In this review, we describe the optimal measures for each level of assistance. Emergency Department: diagnose correctly, adequate analgesia, severity assessment, initiate correct volume replacement. Hospitalization units: clinical and analytical assessment of severity every 12 hours is essential during the first 48 h. If signs of organ failure are present, the patient should be admitted to the Intensive Care unit. The following procedures should be taken: maintain analgesia, appropriate hydration, commence nutrition, measure intra-abdominal pressure and perform radiological tests. The use of antibiotic prophylaxis is not recommended. Indications for surgery: an increase in intra-abdominal pressure in the absence of response to medical treatment, infected necrosis (could be initially managed with minimally invasive measures, step-up approach), intestinal perforation and acute hemorrhage (usually managed by interventional radiology). Conclusions: acute pancreatitis is usually a mild disease, but in its most severe forms it can lead to high mortality and morbidity. The development of a multidisciplinary protocol and the collaboration and coordination of different specialists is imperative for the correct management of these patients.